Med-D: Decentralized Medical Application
Leveraging Blockchain and Self-Sovereign Identity for a Secure Medical Data Sharing Ecosystem.
Project Abstract
Health information management in Thailand is characterized by significant data fragmentation across diverse public and private healthcare providers employing non-interoperable Electronic Health Record (EHR) systems. This systemic lack of integration hinders continuity of care, contributes to diagnostic delays, necessitates redundant investigations, and poses risks associated with incomplete patient histories, such as missing allergy data. This report details the design and prototype implementation of Med-D, a decentralized health record management system proposed to address these challenges within the Thai context.
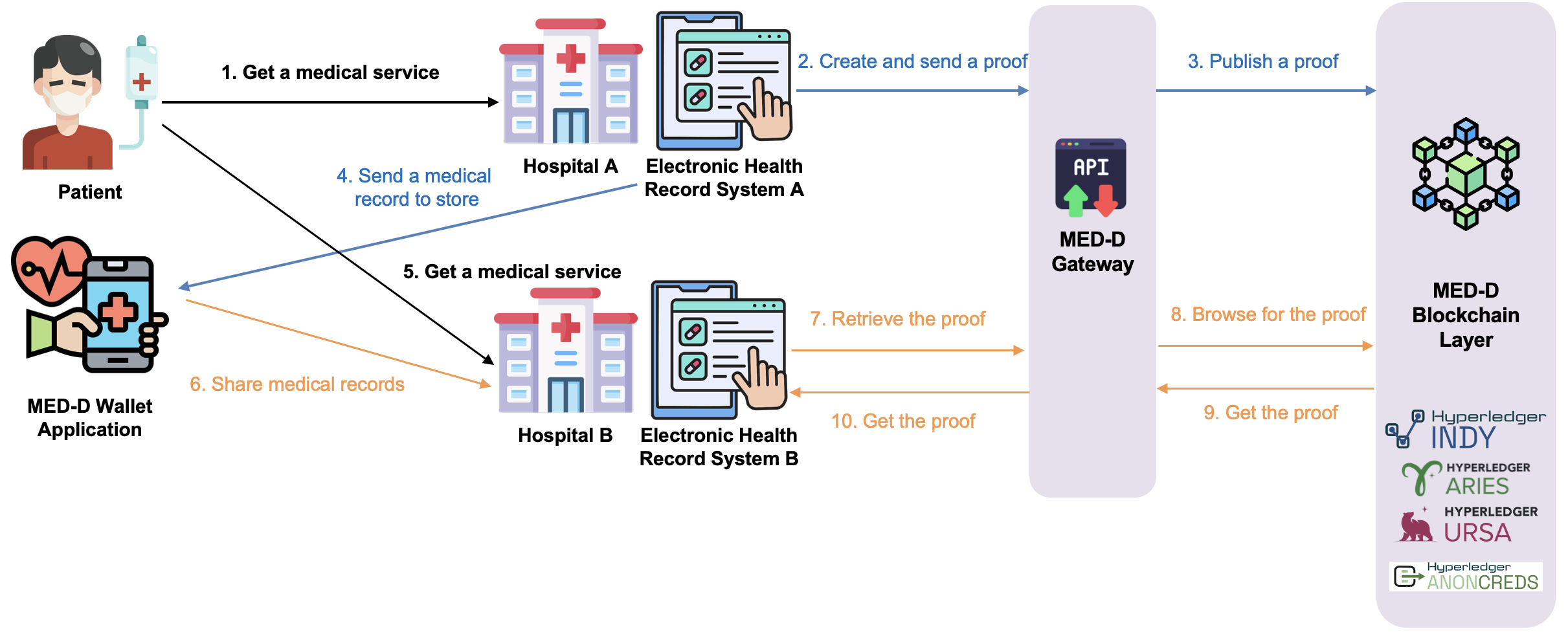
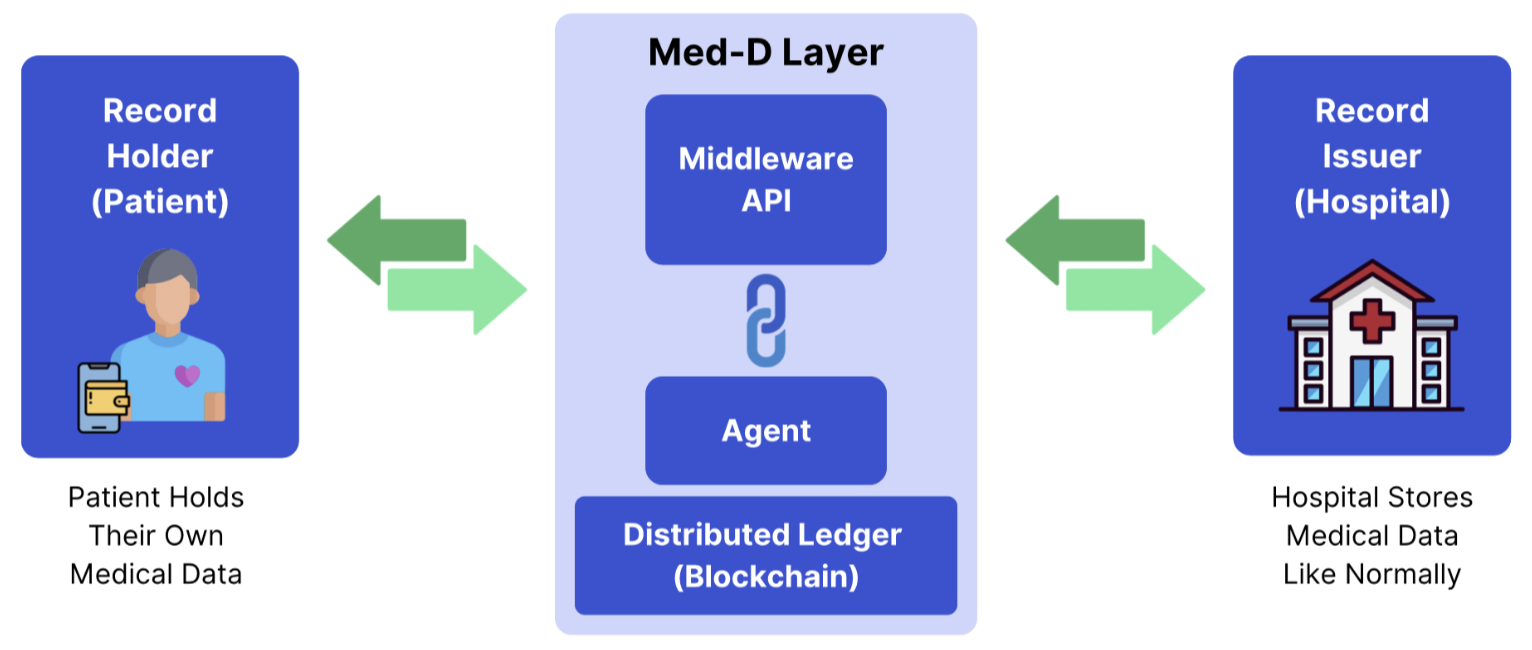
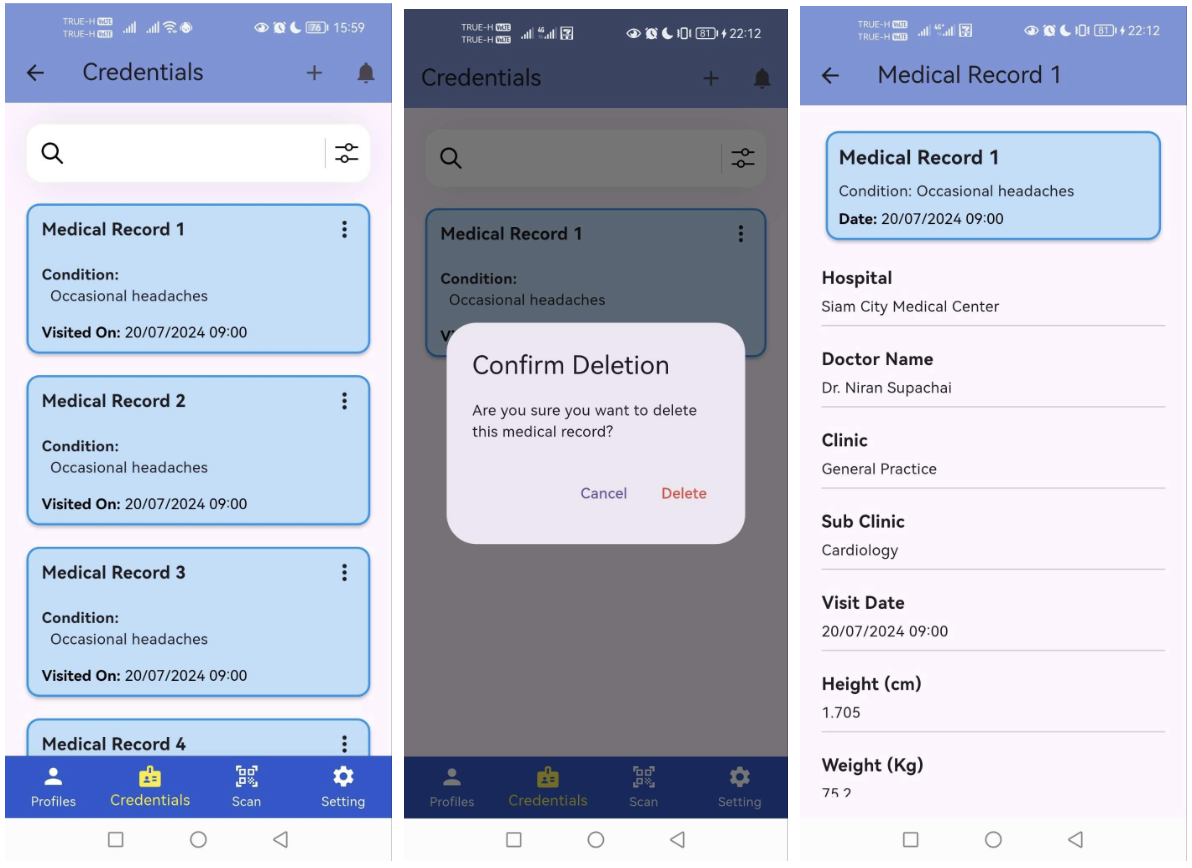
Med-D utilizes W3C Distributed Identifiers (DIDs) for cryptographic identity management of patients and providers, coupled with a simulated blockchain ledger, managed via an Agent service, for storing immutable integrity proofs (SHA-256 hashes) of medical records. A central coordinating API orchestrates key workflows, including DID registration, hash generation during record issuance by simulated EHRs, ledger updates via the Agent, and secure record delivery to a patient-controlled digital Wallet. Furthermore, a verification workflow enables patients to share specific, integrity-verified records with new providers upon consent. The implementation demonstrates the technical feasibility of core Med-D functionalities within a controlled HTTP environment. By promoting data portability, verifiability, and patient control, this architecture offers a potential pathway to mitigate data silos and enhance the efficiency, safety, and patient-centricity of healthcare information exchange in Thailand.
Problem Statement
Thailand's health sector remains characterized by multiple disconnected electronic record systems and paper-based archives, so that patient data is spread across unlinked hospitals, clinics, and private providers. In practice, each facility often uses its own proprietary health information system and data formats. As one Thai expert observes, “there is neither a centralised system nor initiative to streamline all the healthcare data into a single platform like a National EMR system”. Consequently, patient information (e.g., clinical history, medications, test results) is fragmented across silos and even within the same facility, requiring staff to re-enter or reconcile data manually. This fragmentation persists despite broad EHR adoption: a nationwide survey (2011) found only ~50% of hospitals had even basic EHRs, with comprehensive systems in just ~5%, and information sharing between institutions remains limited.
Thailand's 2016 ten-year e-Health Strategy (e.g., “AI Smart Health Profile”) and recent pilots (e.g., Mor Promt personal health record) aim to improve interoperability, but to date no fully integrated, nationwide EHR exists.
Consequences of Fragmentation
- Clinical decision-making and patient safety: Disconnected records severely hamper clinical care. When relevant history is split across systems, providers may miss critical data or duplicate tests. For example, missing allergy or test results stored in a different record can directly harm patients. In theory, health information exchange (HIE) improves safety by reducing errors and eliminating redundant testing, but in Thailand, fragmented systems prevent these gains. Studies show that duplicate or incomplete records lead to missed abnormal findings and treatment errors; Thai experts similarly report that "fragmented databases and software unavailability limit local health data sharing," undermining coordinated care. Without interoperable EHRs, physicians must rely on patient recall or fragmented paper reports, increasing the risk of misdiagnosis and medication errors.
- Administrative burden and operational inefficiency: Fragmentation imposes heavy workload on staff. Without shared systems, each facility duplicates data entry, referral paperwork, and manual record transfer. One study notes that duplicate records alone generate significant costs - for example, time spent locating correct charts, repeating tests, and reconciling files. Conversely, implementing EHRs can streamline workflows: hospitals with mature EHR use have seen shorter patient wait times and higher clinician productivity. In Thailand, however, the disjointed system means clinicians and administrators spend extra hours managing paperwork and cross-checking data. This inefficiency also limits data capture for research and planning: policymakers lack easy access to integrated datasets, hampering epidemiological surveillance
- Limited patient access and engagement: Fragmented data also restricts patient empowerment. Thai patients generally cannot view a single consolidated health record; instead they must obtain printed summaries or digital copies from each provider. The Ministry of Public Health's new “Mor Promt” PHR platform allows patients to retrieve health data from participating providers via an OTP system, but uptake is limited and many facilities are not yet connected. This lack of accessible records undermines preventive care and second opinions. Studies have shown that when patients can easily review their records (e.g., via patient portals), communication improves and medical errors drop. In Thailand's current environment, patients cannot routinely share complete histories between doctors or monitor chronic conditions proactively.
- Prolonged patient wait times: Data silos contribute directly to longer waits for care. When records are not electronically shared, front-line staff must spend extra time retrieving or recreating information at each visit or referral. Studies from other settings have found that mature EHR adoption is associated with decreased waiting times for patients. Thai research similarly notes that implementing a unified digital referral platform “will increase data visibility and accessibility by reducing waiting time”. In practice, fragmented information means longer queues and delays: for example, a referral to a tertiary hospital often involves manual faxed summaries and duplicate testing, lengthening the patient's journey.
Project information
- Category Undergraduate Student Project
- Project date 02 May, 2025
- Team Member Nunthatinn Veerapaiboon, Poon
Thanawin Pattanaphol, Win
Atchariyapat Sirijirakarnjareon, Beam
Petch Suwapun, Diamond - Project Advisor Dr. Charnon Pattiyanon